Pulling, cramp-like pain when walking, which causes you to have to stop and rest is often the first symptom of peripheral arterial disease (PAD). This circulatory disorder, which almost always affects the legs, develops in roughly 20% of people in old age. In severe cases, it can lead to amputation of the affected foot or leg. Minimising risk factors and changing lifestyle are important for treatment and prevention, as well as improving quality of life. And here those affected have the best chance of positively influencing the course of the disease.
What is Peripheral Arterial Disease?

PAD is the progressive narrowing of arteries in the legs (and in rare cases, arms). This leads to a lack of exygen and nutrients being supplied to the tissue in the limbs. The problem with it: In the early stages, the circulatory disorder remains symptom-free - those affected don’t even notice there’s a problem. Only in the second stage does pain start to occur when walking for longer periods. This arises from the insufficient supply of oxygen (ischemic pain). The resulting pain and stopping after a certain walking distance (intermittent claudication, approximately "phased claudication") is a typical symptom and leads to the issue of "claudication”, By which the PAD is commonly known. In the third stage, pain also occurs even when resting, often at night. This results from the lying position, as the blood can no longer flow into the lower leg sections by gravity. This pain can be relieved quickly, albeit temporarily when you sit or let your legs hang down. In the fourth stage of PAD, there is extensive damage to the undersupplied tissue, poorly healing ulcers and even extensive tissue death (necrosis). Often only an operation or, in the worst case, an amputation can help to avoid life-threatening complications.
How does the intermittent claudication "PAOD" develop?
The increasing narrowing of the blood vessels is caused by the accumulation of plaques on the inside of the arteries, known as arteriosclerosis. If the disease progresses untreated, even larger vessels can almost completely close. Plaques often arise as a result of previous damage to the sensitive inner skin of the arteries, which is normally perfectly smooth in its healthy state. This creates rough areas where waste products can accumulate, calcifying over time. These blockages continue to grow, but initially cause no symptoms at all. The main risk factors for this damage to the vascular lining and the formation of plaques are smoking, obesity and high blood pressure. In addition, diseases like diabetes, Lipid metabolism disorders or, more rarely, inflammatory changes in the blood vessels can also contribute to the development of PAOD. In general, older people - especially men - have a higher risk of developing PAD.
How is PAD diagnosed?

There are a number of testing methods that can be used to confirm the diagnosis of PAD:
- Function tests (e.g. treadmill test).
- Control of pulse strength and sensitivity, listening to the hamstrings with the stethoscope.
- Ultrasound examinations.
- Angiography (visualization of blood vessels in an X-ray or CT using an injected contrast agent).
- Laboratory tests of blood samples.
What treatment is available for peripheral arterial disease?
Those affected should definitely see a doctor at the first signs of PAD, because the earlier the primary symptoms are recognised, the more effectively it can be treated. Above all, it is important to eliminate risk factors: Quitting smoking and the treatment of high blood pressure, diabetes or lipid metabolism disorders make a huge contribution. In the early stages, a combination of circulation-boosting drugs, lifestyle changes and exercise therapy is usually successful, though in advanced stages, blood circulation can often only be improved through surgical procedures such as :
- Removal of plaque in the veins (limescale peeling).
- Expansion of narrowed vessel sections.
- Insertion of a tubular implant (stent) that holds a short-length seal open.
- Bypass surgery, such as a leg vein transplant to bypass the narrowed vessel.
The sooner PAD is recognised, the better the chances of being able to avoid surgery. So see a doctor at the first signs!
Prevention and PAD?
Adapting a healthy and active lifestyle will help reduce the risk of PAD. Refraining from cigarettes, alcohol coupled with healthy nutrition, weight reduction and regular endurance sports or targeted exercises for legs and feet are ideally suited.
Can soft insoles help with PAD?

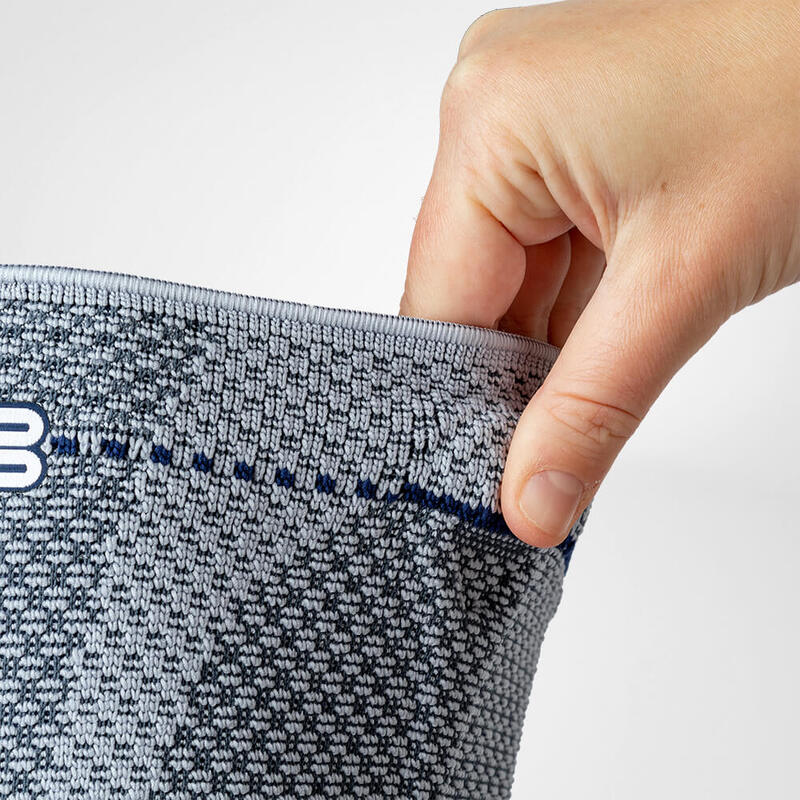
In the advanced stages of PAOD, poor blood flow can lead to wound healing disorders in the legs and feet. Poor healing wounds can be entry points for pathogens resulting in massive infections, ulcers and necrosis. Poorly fitted footwear causing pressure points, blisters or chafed areas should be avoided at all costs for those with PAD. The high quality soft padding ErgoPad soft Diabetes distributes the pressure evenly over the entire running surface of the foot. As a result, it relieves the critical zones on the heel and the base joint of the big toe, which are particularly stressed when loading.
For assistance selecting the right product for your needs, book a video consultation with a Bauerfeind expert: Call us on +971 4 433 5684.